Jaundice is often a symptom of a wide range of diseases of the blood system, liver, biliary tract and gastrointestinal tract. More than 400 reasons are known that cause a pathological increase in the content of bilirubin in the blood plasma – a yellow substance responsible for the unhealthy coloration of the whites of the eyes and skin.
What is jaundice
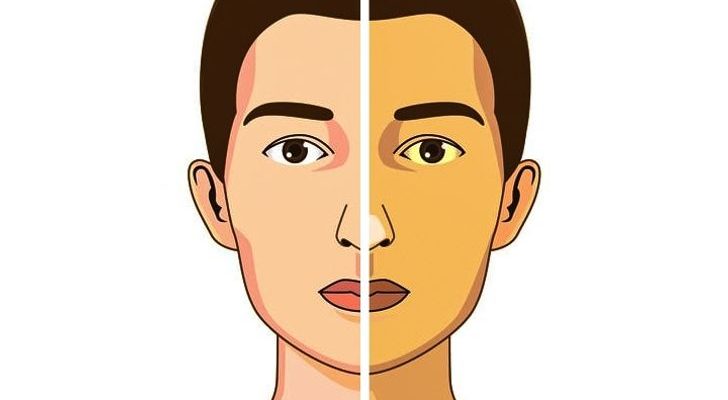
Hyperbilirubinemia or jaundice is a pathological condition that occurs with an increase in the content of bilirubin in the blood plasma. Bilirubin easily enters into chemical interaction with proteins, forming yellow compounds. It is for this reason that the staining of the skin and the whites of the eyes occurs. First of all, yellowness is determined on the sclera, since the albuminous membrane of the eyes contains a lot of elastin – a protein that has the greatest affinity for bilirubin. The skin with jaundice turns yellow later, because the protein collagen, which is abundant in the skin, has a lower affinity for bilirubin.
The mechanism of jaundice, or the pathogenesis of hyperbilirubinemia

Hemoglobin is an oxygen and carbon dioxide carrier protein that provides gas exchange in the human body. Consists of a protein fraction – globin, and heme – a cofactor that determines the function of the compound. The presence of iron atoms in the composition of heme allows hemoglobin to transport oxygen from the lungs to tissues and transport carbon dioxide in the opposite direction. Erythrocytes or red blood cells are almost completely filled with hemoglobin and act as a “truck” for hemoglobin.
The life span of an erythrocyte is approximately three months. After this period, red blood cells are sent to the spleen for disposal. The destruction of red blood cells is accompanied by the release of hemoglobin, which is broken down into globin and heme. Globin metabolism is simple, protein breaks down into individual amino acids. Heme is sequentially cleaved by enzymes to biliverdin, and then to bilirubin (indirect, unbound). This is the suprahepatic stage of heme metabolism.
At the next stage, bilirubin, in connection with blood plasma proteins, is transported to the liver. In the liver, it combines with glucuronic acid and is incorporated into bile. This process is called conjugation and corresponds to the hepatic stage of heme metabolism. After conjugation, bound or direct bilirubin is formed.
Through the bile ducts, bile enters the duodenum, where it is involved in the breakdown of fats. Part of the direct bilirubin that has entered the intestine is transformed into urobilinogen (with the participation of the intestinal microflora), which is reabsorbed into the blood and excreted by the kidneys (gives a yellow color to the urine). The remaining bilirubin is converted to stercobilinogen, which in turn is converted to stercobilin (which gives a dark color to the feces). This is the subhepatic stage of heme metabolism.
Violation of this sequence at any stage leads to an increase in the concentration of blood bilirubin or hyperbilirubinemia. The high toxicity of unbound bilirubin explains a number of complications associated with jaundice. There are over 400 known causes of jaundice.
Types of jaundice
Depending on the level at which the metabolic disorder of bilirubin has occurred, there are three types of hyperbilirubinemia:
Suprahepatic or hemolytic jaundice
Hepatic or parenchymal jaundice
Subhepatic or obstructive jaundice
Causes of jaundice
Suprahepatic or hemolytic jaundice
It occurs with massive hemolysis – a violation of the integrity of erythrocytes. The body does not have time to utilize bilirubin, which is formed from heme, which causes an increase in its level in the blood. As a result of hyperbilirubinemia, yellowness of the skin and mucous membranes is noted. According to this mechanism, jaundice occurs in severe malaria, hereditary diseases of the blood system.
Parenchymal or hepatic jaundice
Parenchymal jaundice is caused by diseases or pathological conditions that affect the function of liver cells (hepatocytes). Under normal conditions, all unbound bilirubin, entering the hepatocyte with the bloodstream, binds to glucuronic acid. As a result, a bound form of bilirubin is formed, which does not possess toxic properties. However, with parenchymal liver diseases accompanied by the death of hepatocytes, such as viral hepatitis and cirrhosis, the organ’s ability to bind indirect bilirubin and neutralize its toxic properties decreases.
Obstructive jaundice
The reason for this form of hyperbilirubinemia is clear from the name. In the event of mechanical blockages in the path of the outflow of bile from the liver, bound bilirubin begins to be absorbed into the blood plasma. Complete obstruction of the biliary tract leads to the appearance of colorless feces, since there are no intermediate forms of bilirubin in the intestine – urobilinogen, stercobilinogen, stercobilin. Despite the absence of urobilinogen in urine, the excess of bound bilirubin makes it look like strong tea or beer. The main cause of obstructive jaundice is gallstones with calculous cholecystitis.
A mechanical block in the biliary tract can lead to a significant increase in the concentration of bilirubin in the blood. At the same time, conditions are created for the loss of its salts into the skin, which explains why patients with this form of hyperbilirubinemia often complain of intolerable itching with jaundice.
Common pathologies with hyperbilirubinemia
Hemolytic hyperbilirubinemia. – Sickle cell anemia (code D57 according to ICD-10);
Thalassemia (D56);
Deficiency of glucose-6-phosphate dehydrogenase (D55);
Pyruvate kinase deficiency (D55.2);
Hereditary spherocytosis (D58);
Autoimmune hemolytic anemia (D59.1);
Drug-induced hemolytic anemias (D59.0);
Other non-autoimmune hemolytic anemias (D59.4);
Gilbert’s syndrome (E80.4);
Hemolytic disease of the newborn (P55);
Kernicterus (P57);
Hepatic hyperbilirubinemia. – Alcoholic liver disease (K70);
Toxic liver damage (K71);
Liver cirrhosis (K74);
Viral hepatitis (B15, B16, B17);
Liver tumors (C22);
Subhepatic hyperbilirubinemia. – Gallstone disease (K80);
Pancreatic cancer (C25);
Biliary atresia (Q44.2);
Cancer of the biliary tract (C22.1);
Acute pancreatitis (K85).
Jaundice in newborns
Jaundice of newborns is a physiological (normal) condition that occurs in newborns in the first weeks of a child’s life. The reason lies in the imperfection of enzyme systems that ensure the breakdown of bilirubin, in combination with increased utilization of the fetal form of hemoglobin, which is characteristic only for the period of intrauterine development.
Physiological jaundice of newborns is diagnosed in about 50-60% of children. With prematurity, this indicator increases. Although this condition is not dangerous, 1 in 40-60 thousand newborns develops nuclear jaundice. This formidable complication is accompanied by impaired brain function due to the high toxicity of indirect bilirubin. Clinically, nuclear jaundice is manifested by pronounced yellowness of the skin and sclera of the eyes, constant crying, lethargy, refusal to breastfeed, fever, and in severe cases, convulsions, coma.
If the above symptoms occur, emergency hospitalization of the child to the neonatal pathology department is necessary. If left untreated, kernicterus can cause permanent brain damage and, in severe cases, death.
The main treatment for neonatal hyperbilirubinemia is phototherapy. Ultraviolet rays transform toxic indirect bilirubin into its water-soluble forms, which are excreted directly through the liver and kidneys. As a result, the level of hyperbilirubinemia is significantly reduced without the use of any medications.
As a prophylaxis against kernicterus, breastfeeding is recommended from the first hours of a child’s life as recommended by a pediatrician or breastfeeding specialist. Overeating can also increase the risk of hyperbilirubinemia in newborns. Sunbathing is recommended during warmer months.
The safe concentration of bilirubin in the blood of newborns is not more than 150 mmol / l. The concentration of indirect bilirubin more than 400 mmol / l leads to necrosis of the brain nuclei.
As a prophylaxis against kernicterus, breastfeeding is recommended from the first hours of a child’s life as recommended by a pediatrician or breastfeeding specialist. Overeating can also increase the risk of hyperbilirubinemia in newborns. Sunbathing is recommended during warmer months.
The safe concentration of bilirubin in the blood of newborns is not more than 150 mmol / l. The concentration of indirect bilirubin more than 400 mmol / l leads to necrosis of the brain nuclei.
Jaundice treatment
Hyperbilirubinemia is most often just a consequence of a particular disease. To eliminate jaundice, treatment of the underlying pathology is necessary. Due to the large number of possible reasons for the increased levels of bilirubin in the blood, doctors in several specialties are involved in this problem.
Hemolytic jaundice mainly refers to diseases of the blood system and is treated by hematologists. Cases of poisoning with hepatotropic toxins, drugs and poisons require the consultation of a toxicologist. Treatment of liver diseases is a specialty of a hepatologist. Liver tumors are treated by oncologists. Subhepatic jaundice, regardless of the cause, requires the consultation of a surgeon (surgeon-oncologist).
Etiotropic therapy of hyperbilirubinemia
Etiotropic therapy is a treatment aimed directly at the cause of the pathology. For example, if a gallstone blocks the outflow of bile, the etiotropic therapy for mechanical hyperbilirubinemia would be surgery to remove the foreign body. Etiotropic therapy is not possible in all cases. Despite the fact that the cause of hemolytic bilirubinemia in hereditary hemolytic anemias is known, there are no treatments that can eliminate the defect in genes that lead to early destruction of red blood cells.
Pathogenetic therapy of hyperbilirubinemia https://en.wikipedia.org/wiki/Bilirubin#Hyperbilirubinemia
Pathogenetic therapy is aimed at individual links of the mechanism leading to the disease or contributing to the deterioration of the patient’s condition. For example, infusion therapy, which uses intravenous fluids of saline or other detoxifying agents, helps remove excess bilirubin through the kidneys.